- Home
- »
- Healthcare IT
- »
-
Population Health Management Market, Industry Report 2033GVR Report cover
![Population Health Management Market Size, Share & Trends Report]()
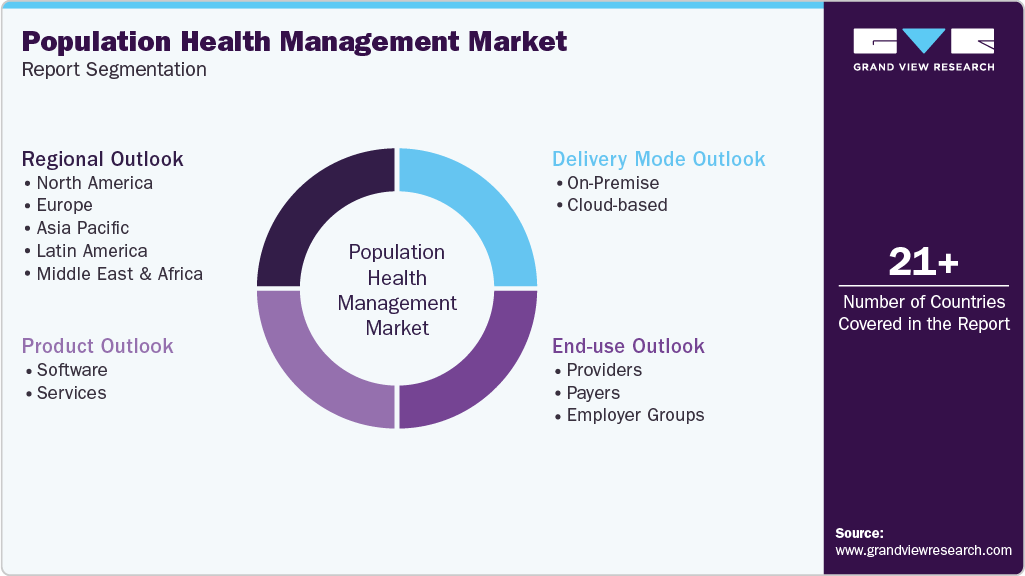
Population Health Management Market (2025 - 2033) Size, Share & Trends Analysis Report By Product (Software, Services), By Delivery Mode (On-Premise, Cloud-based), By End Use (Providers, Payers, Employer Groups), By Region, And Segment Forecasts
- Report ID: GVR-1-68038-187-0
- Number of Report Pages: 150
- Format: PDF
- Historical Range: 2021 - 2023
- Forecast Period: 2025 - 2033
- Industry: Healthcare
- Report Summary
- Table of Contents
- Segmentation
- Methodology
- Download FREE Sample
-
Download Sample Report
Population Health Management Market Summary
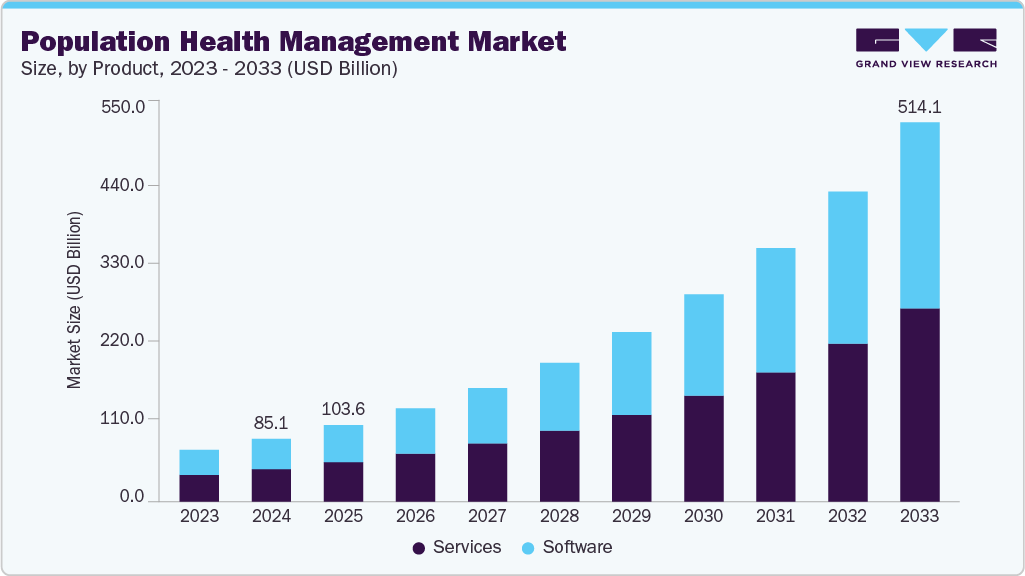
The global population health management market size was estimated at USD 85.15 billion in 2024 and is projected to reach USD 514.12 billion by 2033, growing at a CAGR of 22.2% from 2025 to 2033. The medical industry is rapidly transforming to digitization from a paper-based system, increasing demand for healthcare IT services.
Key Market Trends & Insights
- North America population health management market held the largest share of 46.30% of the global market in 2024.
- The population health management industry in the U.S. is expected to grow significantly over the forecast period.
- Based on product, the services segment held the highest market share of 51.57% in 2024.
- Based on delivery mode, the services segment held the highest market share in 2024.
- By end use, the healthcare providers segment held the highest market share in 2024.
Market Size & Forecast
- 2024 Market Size: USD 85.15 Billion
- 2033 Projected Market Size: USD 514.12 Billion
- CAGR (2025-2033): 22.16%
- North America: Largest market in 2024
- Asia Pacific: Fastest growing market
In addition, increasing demand for solutions supporting healthcare providers has shifted from Fee-For-Service (FFS) to Value-Based Payment (VBP) models. The rising demand for effective disease management strategies is expected to boost market growth. Population Health Management (PHM) has reported significant growth as a systematic, revolutionary, and data-driven approach to enhancing the health and well-being of the population and improving the care experience, ultimately reducing the cost of care. Several countries, including Saudi Arabia, have adopted PHM globally to cater to public health issues.The healthcare industry is increasingly adopting healthcare IT solutions, such as Electronic Health Records (EHRs) and PHM, for value-based compensation. Healthcare providers can benefit from PHM solutions, resulting in financial savings and improved care models. Numerous small & medium-sized healthcare practices and independent physicians lack awareness about EHR and PHM systems. For better clinical outcomes, PHM solutions offer analytics, reporting, and healthcare data integration with EHR systems. Healthcare providers and public health agencies can benefit from data sharing enabled by PHM software.
Furthermore, the transition of the healthcare industry to value-based healthcare from volume-based healthcare has strengthened the approach for incentives around risk reduction, improving outcomes, and appropriate utilization. For most organizations, PHM adoption starts with managing chronic conditions such as cardiovascular diseases, diabetes, and hypertension.
Price Range for Population Health Management Software
Vendor
Pricing Model
Cost Range (USD)
Additional Costs
eClinicalWorks
Subscription
USD 449-USD 25,000/month
Varies based on features and services
Athenahealth
Per provider/month + % of collections
USD 140 + 4%-7% of collections
Varies based on services utilized
Philips
Per user/month
USD 50-USD 8,000/month
Implementation: USD 5,000-USD 200,000+
Arcadia.io
Per user/month
USD 100-USD 60,000/month
Implementation: USD 5,000-USD 50,000
Market Concentration & Characteristics
The chart below illustrates the relationship between industry concentration, industry characteristics, and industry participants. The x-axis represents the level of industry concentration, ranging from low to high. The y-axis represents various industry characteristics, including industry competition, level of partnerships & collaboration activities, degree of innovation, impact of regulations, and regional expansion. The population health management industry is fragmented, with several emerging solutions, and healthcare providers dominating the market. The degree of innovation is high. The level of merger & acquisition activities and the impact of regulations on the industry is moderate. Moreover, the regional expansion of industry is high.
The population health management industry in healthcare experiences a high degree of innovation driven by technological advancements. The increasing adoption of artificial intelligence in PHM to enhance patient engagement, clinical documentation, and hospital administration supports innovations in the market. For instance, in March 2025, a team of Epic alumni launched ProsperityEHR, a cloud-based electronic health record designed to improve operations in behavioral health organizations.
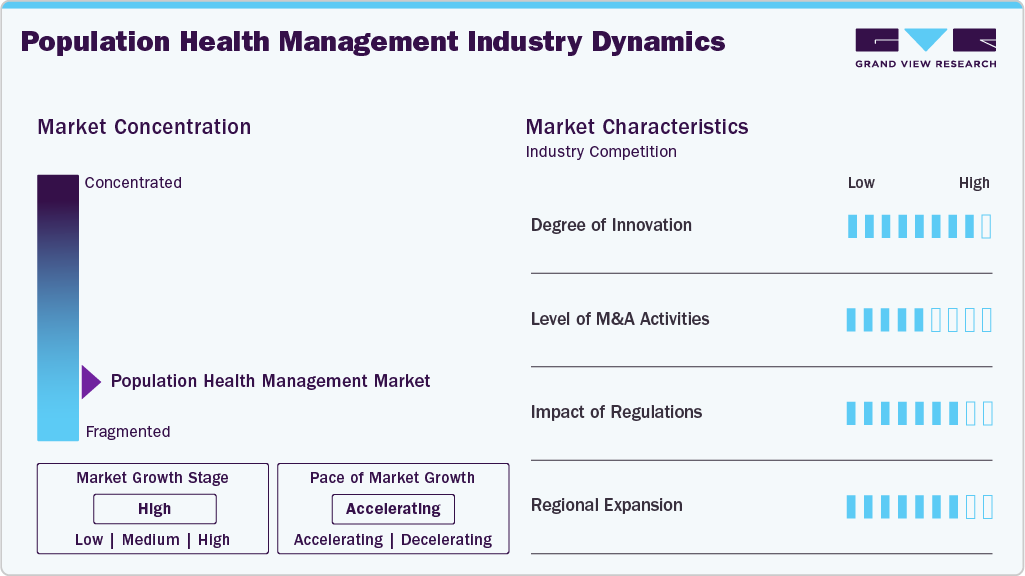
The industry is experiencing a moderate level of partnerships & collaborations undertaken by several key players. This is due to the desire to gain a competitive advantage in the industry, enhance technological capabilities, and consolidate in a rapidly growing market. For instance, in September 2024, HealthEC and VirtualHealth partnered to integrate HealthEC’s advanced population health analytics with VirtualHealth’s HELIOS care management platform.
“We have an outstanding platform that we’ve developed into a single solution for end-to-end medical management. HELIOS is used by big players in both the payer and provider markets because it can support coordinated care management, population health management, utilization management, FHIR interoperability, and more, all in one place. By working with population health analytics leader HealthEC, HELIOS customers will be able to connect population health data on a deeper level and provide insights that lead to improved patient care and health outcomes.”
-Adam Sabloff, Founder and CEO of VirtualHealth
Regulations, such as the HIPAA in the U.S. and the GDPR in Europe, establish standards for safeguarding patient data privacy and security. Compliance with these regulations is crucial for AI applications in healthcare to ensure the safe and secure handling of patient information, reducing the risk of data breaches and unauthorized access.
Companies within the population health management sector seek geographic expansion strategies to maintain their foothold in emerging markets and attract customers from these regions. The industry is witnessing high geographical expansion, driven by an increasing customer base for population health management platforms and solutions. For instance, in June 2024, Pediatric Associates, the largest private pediatric primary care group in the U.S., selected Innovaccer’s AI-driven platform to enhance population health management and value-based care.
Product Insights
Based on product, the services segment held the largest market share of 51.57% in 2024. Demand for PHM services is increasing among hospitals and other healthcare organizations to involve third parties in assessing patient data. The need for integrated healthcare systems also increases demand for PHM services. Besides, rising R&D investment by manufacturers to launch innovative products has supported healthcare organizations to a major extent. For instance, in December 2022, Morris Heights Health Center (MHHC) launched a partnership with Garage, a population health management technology company. Under this partnership, the health center will use a platform to improve care in the Bronx community for 50,000 patients.
Company’s Garage’s Software as a Service population health management platform “Bridge” is designed to connect care teams and healthcare providers to facilitate patient information exchange, secure messaging, patient tracking & communication, referral management, clinical integration, clinical intelligence, clinical data management, and clinical analytics.
The software segment is expected to grow at the fastest CAGR during the forecast period. The primary factor fueling this growth is the increasing adoption of cloud-based analytics platforms and interoperable health information systems, which enable real-time data integration, risk stratification, care coordination, and predictive modeling. Moreover, integrating artificial intelligence (AI), machine learning (ML), and big data analytics within PHM software further enhances its ability to provide actionable insights, thereby empowering healthcare providers to proactively manage patient populations and reduce hospital readmissions.
Delivery Mode Insights
Based on delivery mode, the cloud-based segment held the majority of market share of 72.05% in 2024 and is anticipated to register growth at the highest CAGR during the forecast period. A cloud-based population health management suite improves the process with cutting-edge data integration technologies and advanced analytics, further benefiting end-users in meeting their population health management requirements. In addition, cloud-based platforms assist with workflow automation, improved care management, and coordination with better clinical results.
Furthermore, the demand for cloud-based solutions is rising, leading to acquisitions and mergers to offer cloud-based solutions. This trend transforms the market, improving efficiency and care delivery. For instance, in May 2020, Koninklijke Philips N.V. acquired Vital Health to enable the development of cloud-based PHM solutions.
End Use Insights
Healthcare providers held a 47.63% share of overall revenue in 2024, owing to improved clinical outcomes by aiding in better disease management, reducing inpatient stays, and minimizing physician observation hours. Healthcare providers are increasingly investing in population health management to offer better outcomes. It tracks discharged patients’ vital signs, which are then analyzed to provide insights into their health.
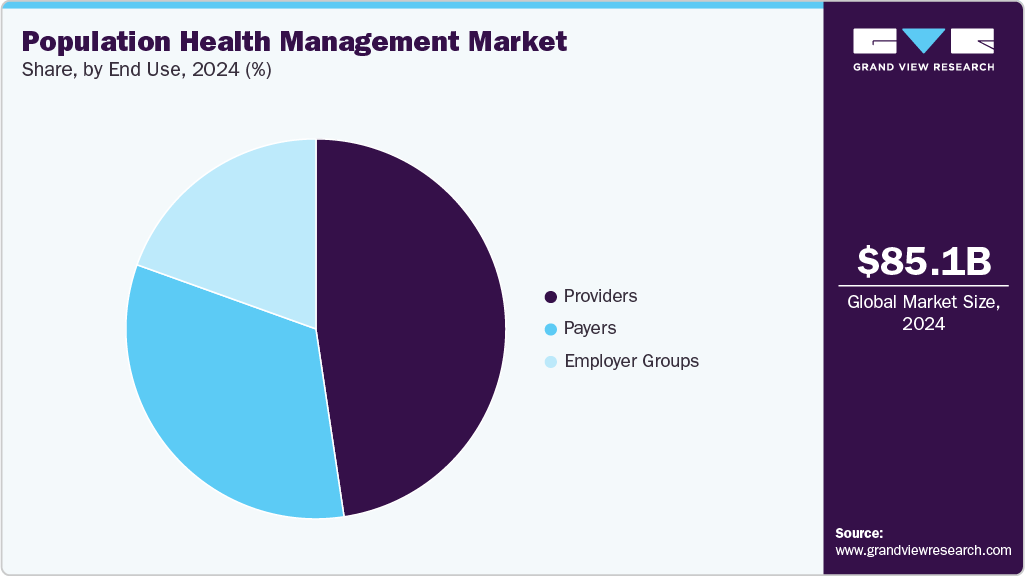
The employer groups segment is expected to grow fastest over the forecast period. The influence of employment on an individual's health varies depending on the nature of the job and the workplace environment, which significantly contributes to health inequality. As most employees work in the private sector, health and wellness policies implemented by private organizations considerably influence health outcomes across Integrated Care Systems (ICSs).
Regional Insights
North America dominated the market with the largest revenue share of 46.30% in 2024. This growth is attributed to supportive government regulations for healthcare IT, high disposable incomes, and a high geriatric population in the U.S. & Canada. The strategic presence of major players, such as Optum, Inc., and Veradigm LLC, and the government's adoption of PHM programs are among the key factors responsible for the market growth in the region.

U.S. Population Health Management Market Trends
The population health management market in the U.S. held the largest market share in 2024. The growth of PHM in the U.S. is predominantly driven by the country’s Affordable Care Act (ACA) trend toward value-based care, which results in the advancement of big data capabilities, increased focus on preventive care and personalized medicine, enhancement of healthcare IT structure, and adoption of healthcare IT solutions such as Electronic Medical Records (EMR) and Health Information Exchange (HIE).
Europe Population Health Management Market Trends
The population health management market in Europe is expected to witness significant growth owing to the rapid technological advancements and increasing spending capacity of the people. Europe is one of the most developed regions in the world. However, healthcare IT infrastructure varies widely across Europe. Germany, the UK, France, Italy, and Spain are major countries contributing to the European PHM market. Increasing public & private investments in R&D and the presence of a large number of Healthcare providers are some of the key factors expected to boost the market growth.
The UK population health management market is expected to grow over the forecast period. Rising elective waiting times, an aging population, and growing demand for value-based healthcare delivery are among the key factors driving the market. The NHS in the UK is transitioning from a competitive healthcare model to a collaborative one with the introduction of ICSs and STPs, fueling market growth. Moreover, the UK government and NHS are launching several programs and policies that are expected to create opportunities for PHM providers. For instance, in July 2022, the UK parliament passed the Health and Care Bill, granting legal responsibilities and statutory footing to ICSs, which is expected to directly impact PHM.
The population health management market in Germany is expected to grow significantly over the forecast period, owing to increasing investments in healthcare technology and robust healthcare infrastructure.
Asia Pacific Population Health Management Market Trends
The population health management market in Asia Pacific is projected to experience significant growth in the coming years. The rise in healthcare consumerism, the adoption of digital health technologies, & the increasing prominence of medical tourism establish the foundation for PHM in the region.
Japan population health management market is expected to grow significantly over the forecast period. Rising prevalence of chronic diseases, increasing demand for personalized healthcare solutions, and the growing adoption of artificial intelligence in healthcare contribute to market growth. In addition, technological advancements and growing government support and initiatives further fuel market growth.
The population health management market in China is expected to grow rapidly, owing to the increasing healthcare expenditure and rapid adoption of healthcare IT solutions. Moreover, increasing public and private funding and initiatives propel market growth further.
Latin America Population Health Management Market Trends
The population health management market in Latin America is anticipated to grow at a significant CAGR over the forecast period. This is attributed to the growing awareness about healthcare IT, increasing government spending, and growing advancements in healthcare infrastructure.
Middle East and Africa Population Health Management Market Trends
The population health management market in the Middle East and Africa is expected to grow significantly over the forecast period. The market is characterized by a dynamic landscape driven by the growing adoption of healthcare IT solutions, increasing healthcare expenditures, and supportive government policies. Significant integration of AI in healthcare technology across the region contributes to market growth further.
Key Population Health Management Company Insights
Key players operating in the market are undertaking various initiatives to strengthen their market presence and increase the reach of their products and services. Strategies such as new product launches and partnerships play a key role in propelling the market growth.
Key Population Health Management Companies:
The following are the leading companies in the population health management market. These companies collectively hold the largest market share and dictate industry trends.
- Veradigm LLC
- Oracle
- Conifer Health Solutions, LLC
- eClinicalWorks
- Enli Health Intelligence (Cedar Gate Technologies)
- McKesson Corporation
- Medecision
- Optum, Inc.
- Koninklijke Philips N.V.
- Athenahealth, Inc.
- Welltok (Virgin Pulse)
Recent Developments
-
In January 2025, Percipio Health launched an AI-powered population health platform, securing USD 20 million in Series A funding led by UPMC Enterprises, WAVE Ventures, and Labcorp. The platform uses a smartphone app to collect vision-based and vocal AI biomarkers and other health signals, enabling real-time, device-free, holistic health monitoring and predictive insights for value-based care.
-
In November 2024, Emory Healthcare and Emory Healthcare Network launched a population health collaborative with GuideHealth, an AI-enabled value-based care services company. The collaboration will focus on value-based care for over 350,000 individuals in Georgia.
-
In September 2024, AssureCare launched a real-time integration feature for its MedCompass platform, enabling seamless submission of prior authorization requests directly from EHRs. This advancement ensures compliance with CMS regulations, streamlining the prior authorization process and reducing administrative burdens for payors, ultimately enhancing efficiency in healthcare operations.
-
In June 2024, Zyter|TruCare launched version 24.1, enhancing population health management with advanced care management tools, streamlined authorization and appeals processes, and integrated virtual health features. The update improves patient engagement, operational efficiency, and care coordination, supporting value-based care with analytics, remote monitoring, and seamless interoperability for healthcare organizations.
Population Health Management Market Report Scope
Report Attribute
Details
Market size value in 2025
USD 103.63 billion
Revenue forecast in 2033
USD 514.12 billion
Growth rate
CAGR of 22.2% from 2025 to 2033
Base year for estimation
2024
Historical data
2021 - 2023
Forecast period
2025 - 2033
Report updated
June 2025
Quantitative units
Revenue in USD million/billion and CAGR from 2025 to 2033
Report coverage
Revenue forecast, company ranking, competitive landscape, growth factors, and trends
Segments covered
Product, delivery mode, end use, region
Regional scope
North America; Europe; Asia Pacific; Latin America; MEA
Country scope
U.S.; Canada; Mexico; UK; Germany; France; Italy; Spain; Sweden; Norway; Denmark; Japan; China; India; Australia; Thailand; South Korea; Brazil; Argentina; South Africa; Saudi Arabia; UAE; Kuwait
Key companies profiled
Veradigm LLC.; Oracle; Conifer Health Solutions, LLC; eClinicalWorks; Enli Health Intelligence (Cedar Gate Technologies); McKesson Corporation; Medecision; Optum, Inc.; Koninklijke Philips N.V.; Athenahealth, Inc.; Welltok (Virgin Pulse)
Customization scope
Free report customization (equivalent up to 8 analyst’s working days) with purchase. Addition or alteration to country, regional & segment scope.
Global Population Health Management Market Report Segmentation
This report forecasts revenue growth and provides an analysis of the latest trends in each of the sub-segments from 2021 to 2033. For this report, Grand View Research has segmented the global population health management market based on delivery mode, end use, and region.
-
Product Outlook (Revenue, USD Million, 2021 - 2033)
-
Software
-
Services
-
-
Delivery Mode Outlook (Revenue, USD Million, 2021 - 2033)
-
On-Premise
-
Cloud-based
-
-
End-use Outlook (Revenue, USD Million, 2021 - 2033)
-
Providers
-
Payers
-
Employer Groups
-
-
Regional Outlook (Revenue, USD Million, 2021 - 2033)
-
North America
-
U.S.
-
Canada
-
Mexico
-
-
Europe
-
UK
-
Germany
-
France
-
Italy
-
Spain
-
Sweden
-
Norway
-
Denmark
-
-
Asia Pacific
-
Japan
-
China
-
India
-
Australia
-
Thailand
-
South Korea
-
-
Latin America
-
Brazil
-
Argentina
-
-
Middle East & Africa
-
South Africa
-
Saudi Arabia
-
UAE
-
Kuwait
-
-
Frequently Asked Questions About This Report
b. The global population health management market size was estimated at USD 85.15 billion in 2024 and is expected to reach USD 103.63 billion in 2025.
b. The global population health management market is expected to grow at a compound annual growth rate of 22.16% from 2025 to 2033 to reach USD 514.12 billion by 2033.
b. North America dominated the population health management market with a share of 46.30% in 2024. This is attributable to the supportive government initiatives, rising healthcare costs, and local presence of major players in the market.
b. Some key players operating in the population health management market are Veradigm LLC, Oracle, Conifer Health Solutions, LLC, eClinicalWorks, Enli Health Intelligence, McKesson Corporation, Medecision, Optum, Inc., Advisory Board, Koninklijke Philips N.V., Athenahealth, Inc., Welltok
b. Key factors that are driving the population health management market growth include the shift from Fee-For-Service (FFS) to Value-Based Payment (VBP) models, accelerating demand for healthcare IT solutions, and growing need for disease management strategies.
Share this report with your colleague or friend.
Need a Tailored Report?
Customize this report to your needs — add regions, segments, or data points, with 20% free customization.

ISO 9001:2015 & 27001:2022 Certified
We are GDPR and CCPA compliant! Your transaction & personal information is safe and secure. For more details, please read our privacy policy.
Trusted market insights - try a free sample
See how our reports are structured and why industry leaders rely on Grand View Research. Get a free sample or ask us to tailor this report to your needs.